MIT researchers find a drug that helps erase traumatic memories in mice.
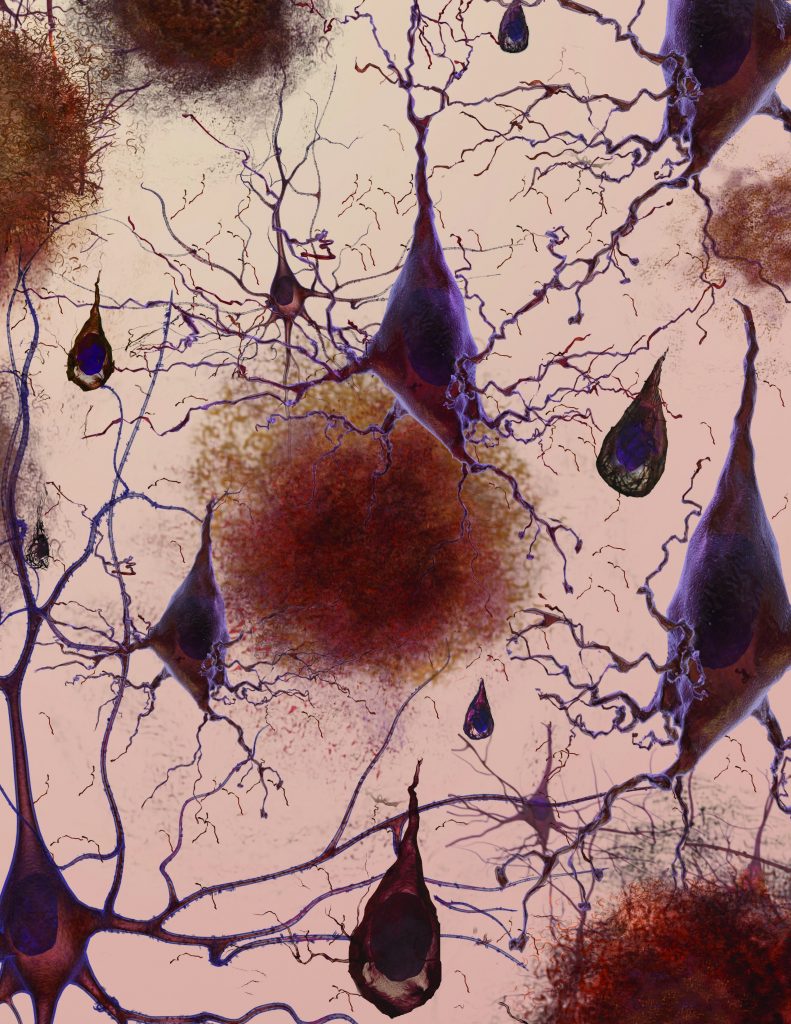
For years, neuroscientist Li-Huei Tsai has been unraveling the brain circuits that underlie memory, searching for approaches that might be helpful in treating Alzheimer’s disease. In 2007, the Massachusetts Institute of Technology scientist identified an experimental drug that could restore lost memories in mice. Lately, she has been wondering whether that kind of drug might be useful to help people forget traumatic events that cause fear and anxiety.
In a study published Thursday in the journal Cell, Tsai and colleagues used a single dose of the drug, called an HDAC inhibitor, to help mice extinguish a fearful memory of a traumatic event that took place in the distant past.
By Carolyn Y. Johnson / Globe Staff