Five volunteers continued receiving 40Hz stimulation for around two years after an early-stage MIT clinical study. Those who had late-onset Alzheimer’s performed significantly better on several assessments than comparable Alzheimer’s patients outside the trial
A new research paper documents the outcomes of five volunteers who continued to receive 40Hz light and sound stimulation for around two years after participating in an MIT early-stage clinical study of the potential Alzheimer’s disease therapy. The results show that for the three participants with late-onset Alzheimer’s disease, several measures of cognition remained significantly higher than comparable Alzheimer’s patients in national databases. Moreover, in the two late-onset volunteers who donated plasma samples, levels of Alzheimer’s biomarker tau proteins were significantly decreased.
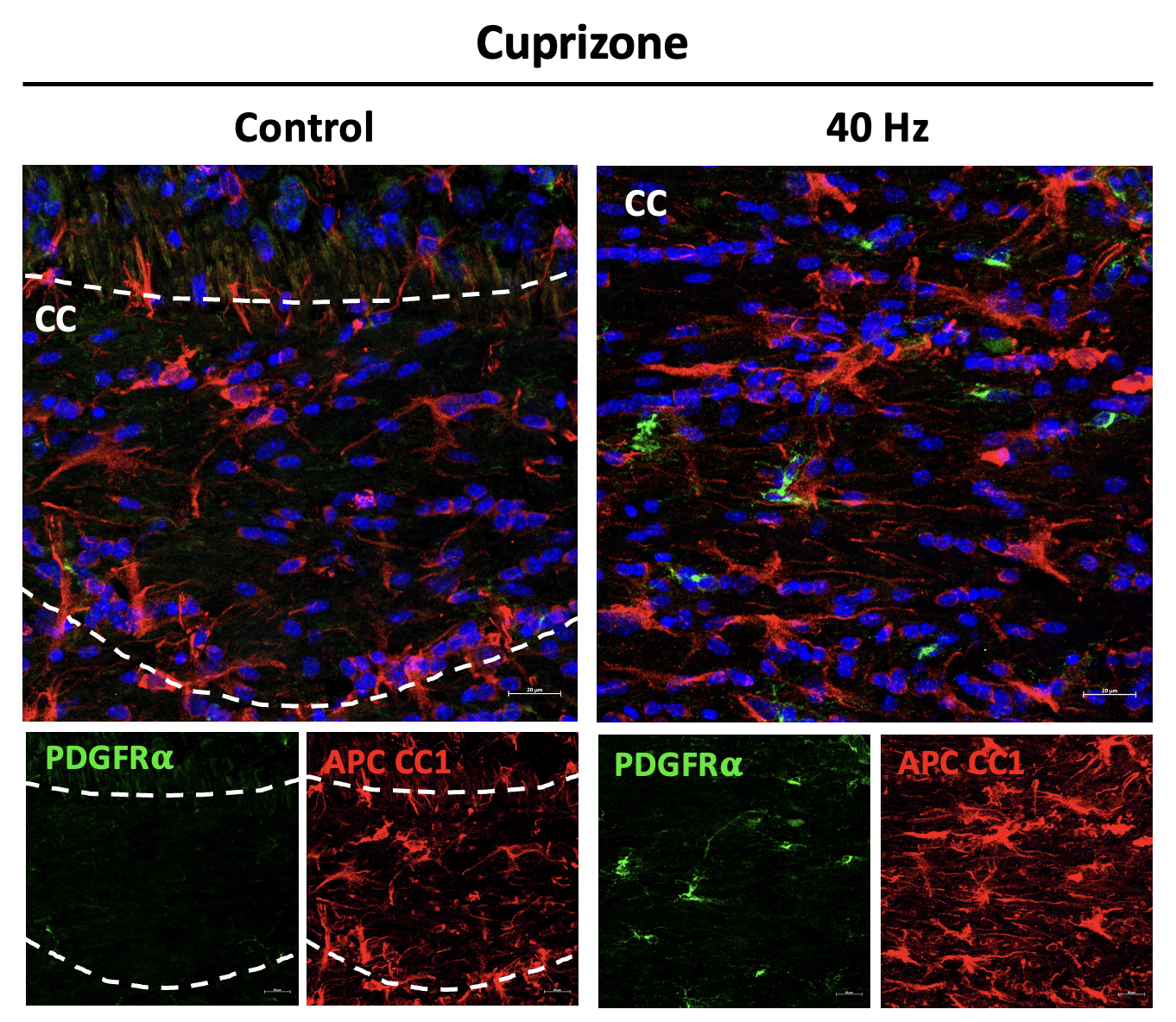
The three volunteers who experienced these benefits were all female. The two other participants, each of whom were males with early-onset forms of the disease, did not exhibit significant benefits after two years. The dataset, while small, represents the longest-term test so far of the safe, non-invasive treatment method (called GENUS, for gamma entrainment using sensory stimuli), which is also being evaluated in a nationwide clinical trial run by MIT-spinoff company Cognito Therapeutics.
“This pilot study assessed the long-term effects of daily 40Hz multimodal GENUS in patients with mild AD,” the authors wrote in Alzheimer’s & Demetntia: The Journal of the Alzheimer’s Association. “We found that daily 40Hz audiovisual stimulation over 2 years is safe, feasible, and may slow cognitive decline and biomarker progression, especially in late-onset AD patients.”
Diane Chan, a former research scientist in The Picower Institute for Learning and Memory and a neurologist at Massachusetts General Hospital, is the study’s lead and co-corresponding author. Picower Professor Li-Huei Tsai, director of The Picower Institute and the Aging Brain Initiative at MIT, is the study’s senior and co-corresponding author.
An “open label” extension
In 2020, MIT enrolled 15 volunteers with mild Alzheimer’s disease in an early-stage trial to evaluate whether an hour a day of 40Hz light and sound stimulation, delivered via an LED panel and speaker in their homes, could deliver clinically meaningful benefits. Several studies in mice had shown that the sensory stimulation increases the power and synchrony of 40Hz gamma frequency brain waves, preserves neurons and their network connections, reduces Alzheimer’s proteins such as amyloid and tau, and sustains learning and memory. Several independent groups have also made similar findings over the years.
MIT’s trial, though cut short by the Covid-19 pandemic, found significant benefits after three months. The new study examines outcomes among five volunteers who continued to use their stimulation devices on an “open label” basis for two years. These volunteers came back to MIT for a series of tests 30 months after their initial enrollment. Because four participants started the original trial as controls (meaning they initially did not receive 40Hz stimulation), their open label usage was six to 9 months shorter than the 30-month period.
The testing at 0, 3 and 30 months of enrollment included measurements of their brain wave response to the stimulation, MRI scans of brain volume, measures of sleep quality and a series of five standard cognitive and behavioral tests. Two participants gave blood samples. For comparison to untreated controls, the researchers combed through three national databases of Alzheimer’s patients, matching thousands of them on criteria such as age, gender, initial cognitive scores, and retests at similar timepoints across a 30-month span.
Outcomes and outlook
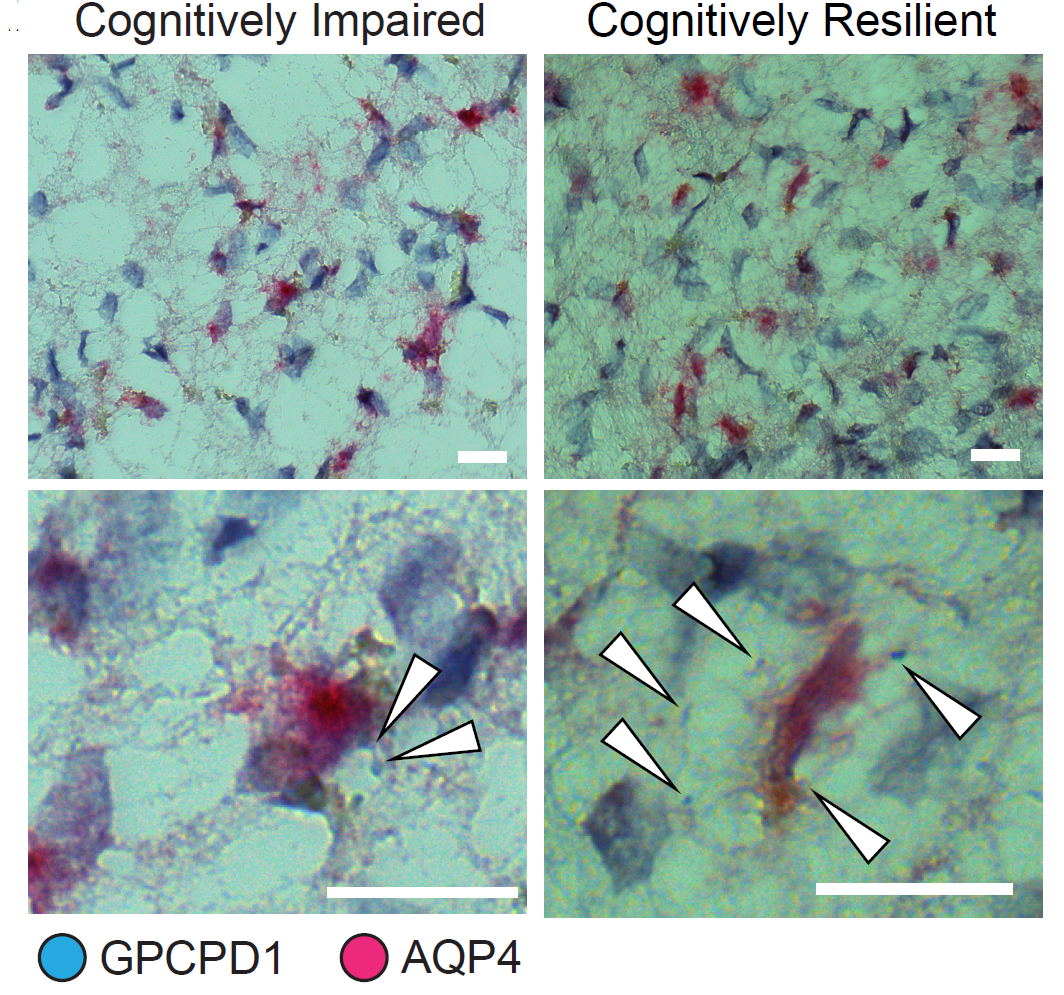
The three female late-onset Alzheimer’s volunteers showed improvement or slower decline on most of the cognitive tests, including significantly positive differences compared to controls on three of them. These volunteers also showed increased brain-wave responsiveness to the stimulation at 30 months and showed improvement in measures of circadian rhythms. In the two late-onset volunteers who gave blood samples, there were significant declines in phosphorylated tau (47 percent for one and 19.4 percent for the other) on a test recently approved by the FDA as the first plasma biomarker for diagnosing Alzheimer’s.
“One of the most compelling findings from this study was the significant reduction of plasma pTau217, a biomarker strongly correlated with AD pathology, in the two late-onset patients in whom follow-up blood samples were available,” the authors wrote in the journal. “These results suggest that GENUS could have direct biological impacts on Alzheimer’s pathology, warranting further mechanistic exploration in larger randomized trials.”
Though the initial trial results showed preservation of brain volume at 3 months among those who received 40Hz stimulation, that was not significant at the 30-month timepoint. And the two male early-onset volunteers did not show significant improvements on cognitive test scores. Notably, the early onset patients showed significantly reduced brain-wave responsiveness to the stimulation.
Though the sample is small, the authors hypothesize that the difference between the two sets of patients is likely attributable to the difference in disease onset rather than the difference in gender.
“GENUS may be less effective in early onset Alzheimer’s disease patients, potentially owing to broad pathological differences from late-onset Alzheimer’s disease that could contribute to differential responses,” the authors wrote. “Future research should explore predictors of treatment response, such as genetic and pathological markers.”
Currently, the research team is studying whether GENUS may have a preventative effect when applied before disease onset. The new trial is recruiting participants aged 55+ with normal memory who have or had a close family member with Alzheimer’s disease, including early-onset.
In addition to Chan and Tsai, the paper’s other authors are Gabrielle de Weck, Brennan L. Jackson,, Ho-Jun Suk, Noah P. Milman, Erin Kitchener, Vanesa S. Fernandez Avalos, MJ Quay, Kenji Aoki, Erika Ruiz, Andrew Becker, Monica Zheng, Remi Philips, Rosalind Firenze, Ute Geigenmüller, Bruno Hammerschlag, Steven Arnold, Pia Kivisäkk, Michael Brickhouse, Alexandra Touroutoglou, Emery N. Brown, Edward S. Boyden, Bradford C. Dickerson and, Elizabeth B. Klerman.
Funding for the research came from the Freedom Together Foundation, the Robert A. and Renee E. Belfer Family Foundation, the Eleanor Schwartz Charitable Foundation, the Dolby Family, Che King Leo, Amy Wong and Calvin Chin, Kathleen and Miguel Octavio, the Degroof-VM Foundation, the Halis Family Foundation, Chijen Lee, Eduardo Eurnekian, Larry and Debora Hilibrand, Gary Hua and Li Chen, Ko Han Family, Lester Gimpelson, David B Emmes, Joseph P. DiSabato and Nancy E. Sakamoto, Donald A. and Glenda G. Mattes, the Carol and Gene Ludwig Family Foundation, Alex Hu and Anne Gao, Elizabeth K. and Russell L. Siegelman, the Marc Haas Foundation, Dave and Mary Wargo, James D. Cook, and the Nobert H. Hardner Foundation.